


slide1 - copy
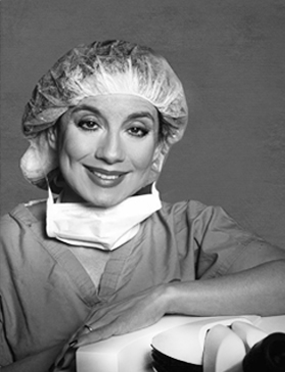
Premier Personalized Eye Care
"America's Most Trusted Eye Doctor"
slide2
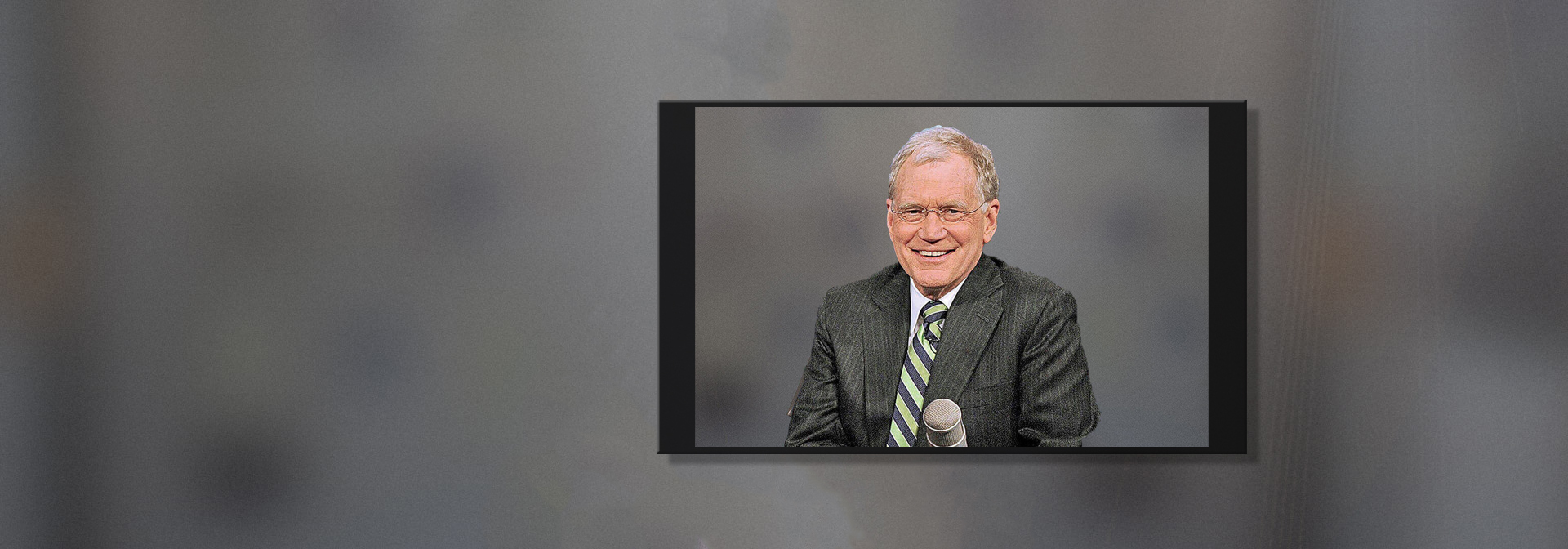
They saved my vision,
and they do a wonderful
job over there!
and they do a wonderful
job over there!
–David Letterman
slide3
“Dr. Belmont,
Thank you so much.
I can see, thanks
to you!”
Thank you so much.
I can see, thanks
to you!”
–Regis Philbin
slide4
"Dr. Sandra Belmont,
whose incredible
skill allows me to
see a million sunsets."
whose incredible
skill allows me to
see a million sunsets."
–Mandy Patinkin, Star of ‘Homeland.’
slide5
"This is the best thing
I’ve ever done."
I’ve ever done."
–Colin Quinn,
Actor and Comedian